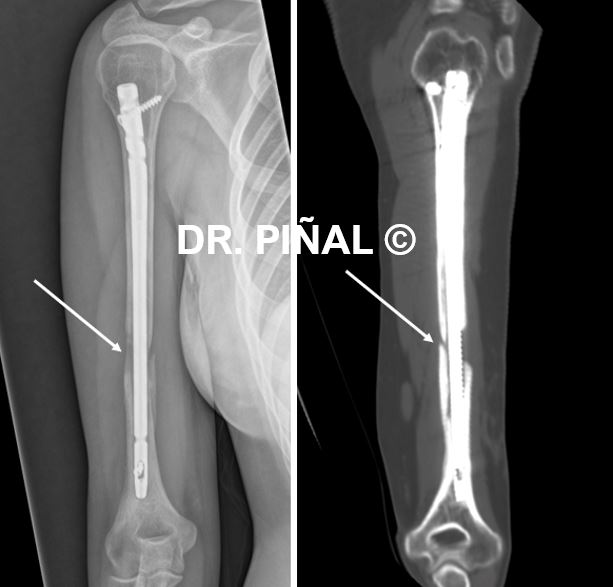
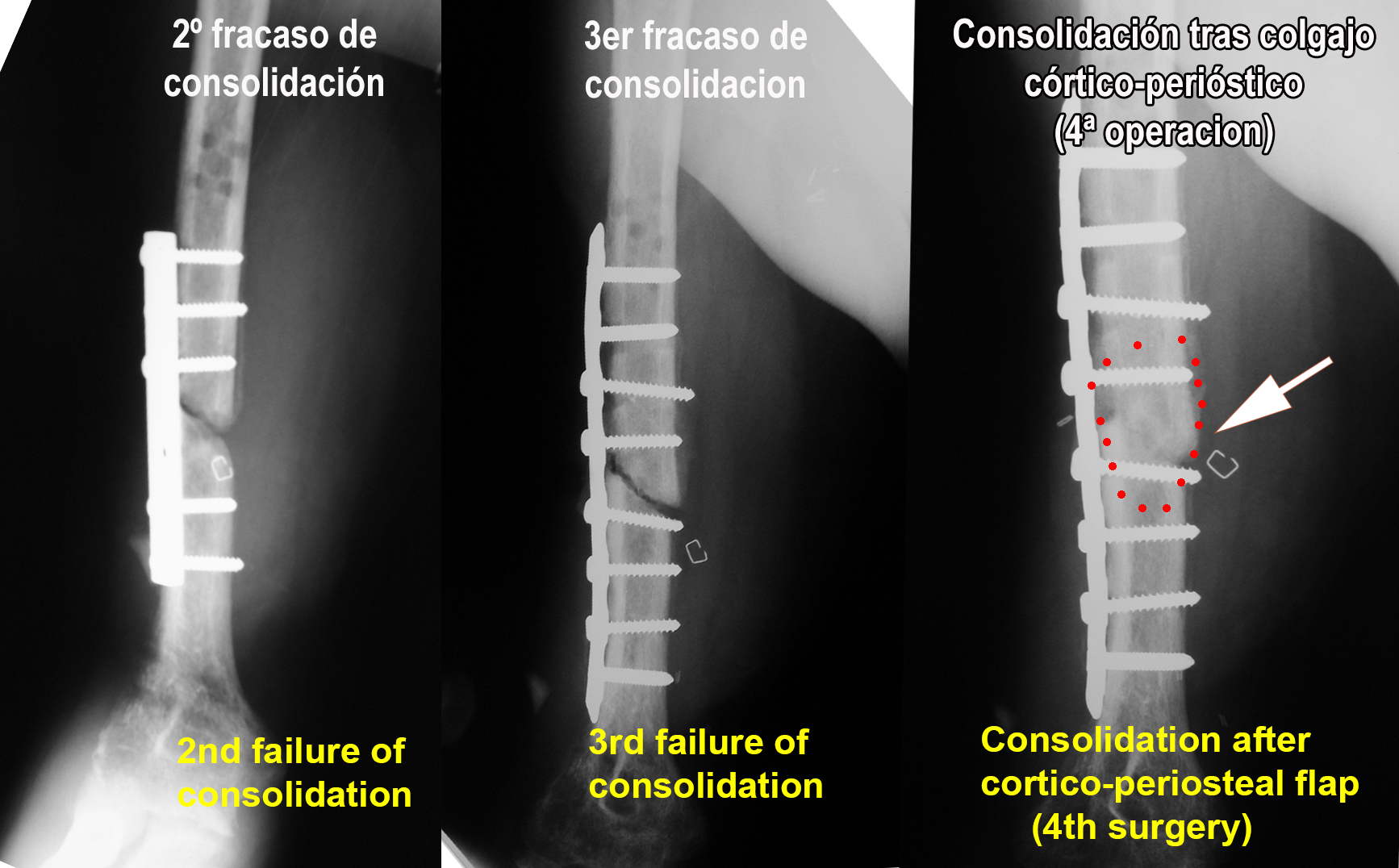
The 20-year-old patient suffered an unconsolidated right humerus fracture with radial nerve injury one year before coming into contact with Dr. Piñal. Despite the modifications in the synthesis in two previous surgeries, the fracture had not been able to consolidate. On the contrary, in recent months the young woman had begun to suffer pain from the bone malunion.
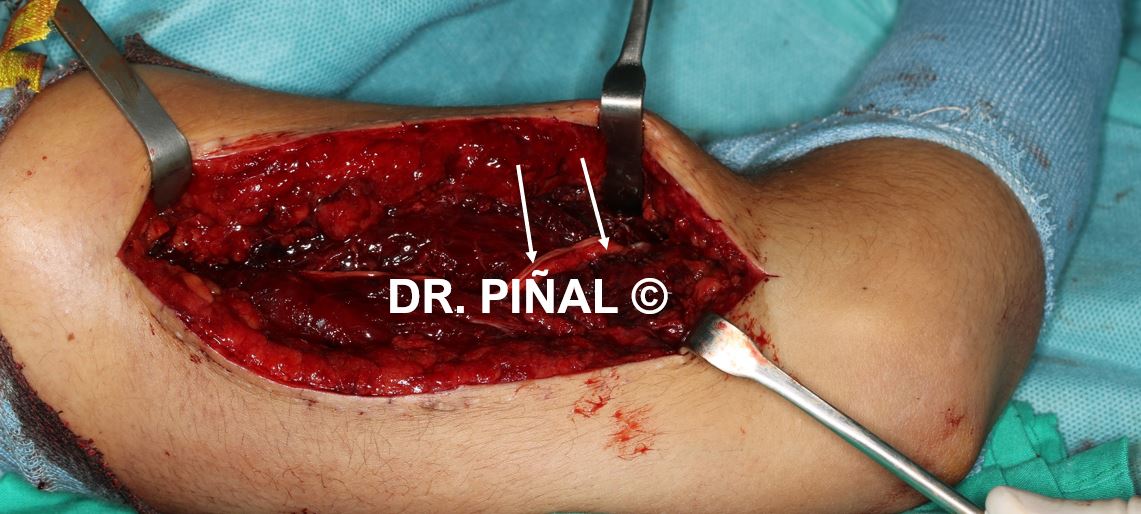
Faced with the threat of failure of the osteosynthesis material with which the patient arrives, Dr. Piñal urgently schedules the microsurgical transfer of a vascularized periosteal flap taken from the internal face of the femur (the periosteum is the fibrous sheath that provides coverage to the bones. It includes the blood vessels that guarantee their nutrition and their capacity to generate bone).

There are fractures that cannot heal because the bed does not have the capacity to do so and the patient is doomed to multiple unsuccessful operations. This occurs in fibrosis due to high-energy fractures, crushing, and multi-surgery cases, or more frequently, all of these factors combined. The end result is that by not healing the bone, the osteosynthesis material “fatigue” and breaks.
Microsurgery allows changing the characteristics of any scar bed, providing scar-free and well vascularized tissue. In long bones, microvascular periosteal flaps also have the intrinsic ability to generate bone and therefore to cause the fracture to consolidate, even in situations where the bed is exhausted. As in the case at hand, it is crucial to intervene before the osteosynthesis material breaks: pain is an imminent sign that this is going to happen, since it indicates micro movements.
The problem
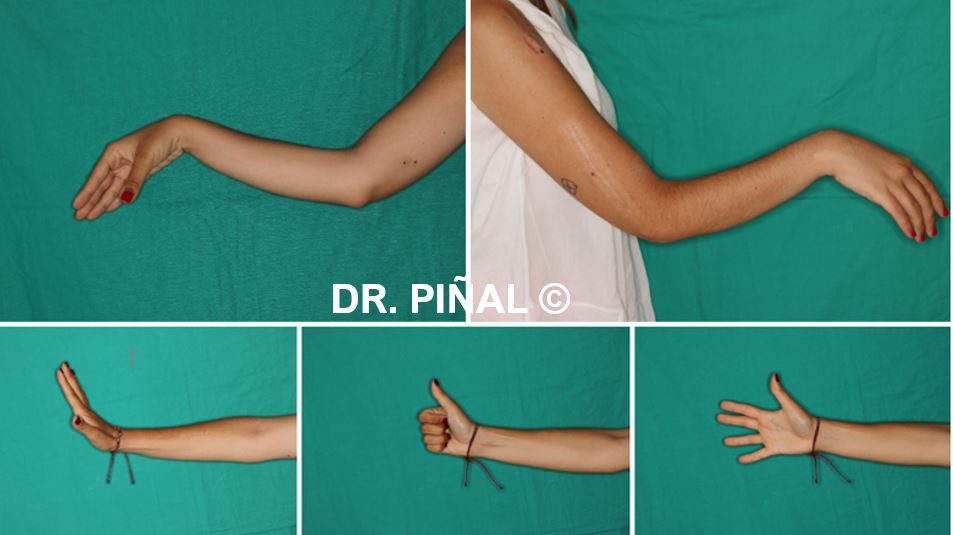
The patient starts from a situation of complete radial paralysis and an atrophic pseudarthrosis of the humerus, accompanied by an extensive bone defect in its anterior region. In turn, the radial nerve is interrupted by approximately 12 cm. The condition causes pain and severe functional limitations to the patient.
The goals
The main objective of Dr. Piñal and his surgical unit is to achieve an adequate synthesis of the fractured area, improving its vascularization and incorporating the ability to generate bone, thus facilitating consolidation. In this way, pain is eliminated and functional recovery is possible.
The plan
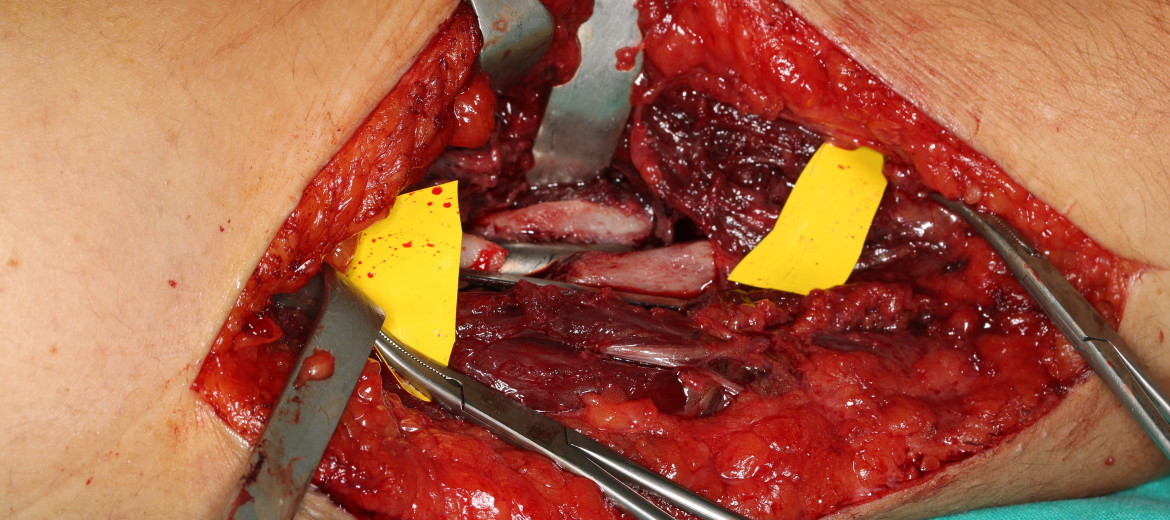
Dr. Piñal designs a microsurgical procedure that begins with the debridement of the pseudarthrosis focus. Once it has been refreshed, he takes the right femoral cortico-periosteal flap from the internal face of the femur, applying it to the anterior face of the humerus and connecting it to the vessels of the arm by anastomosis.
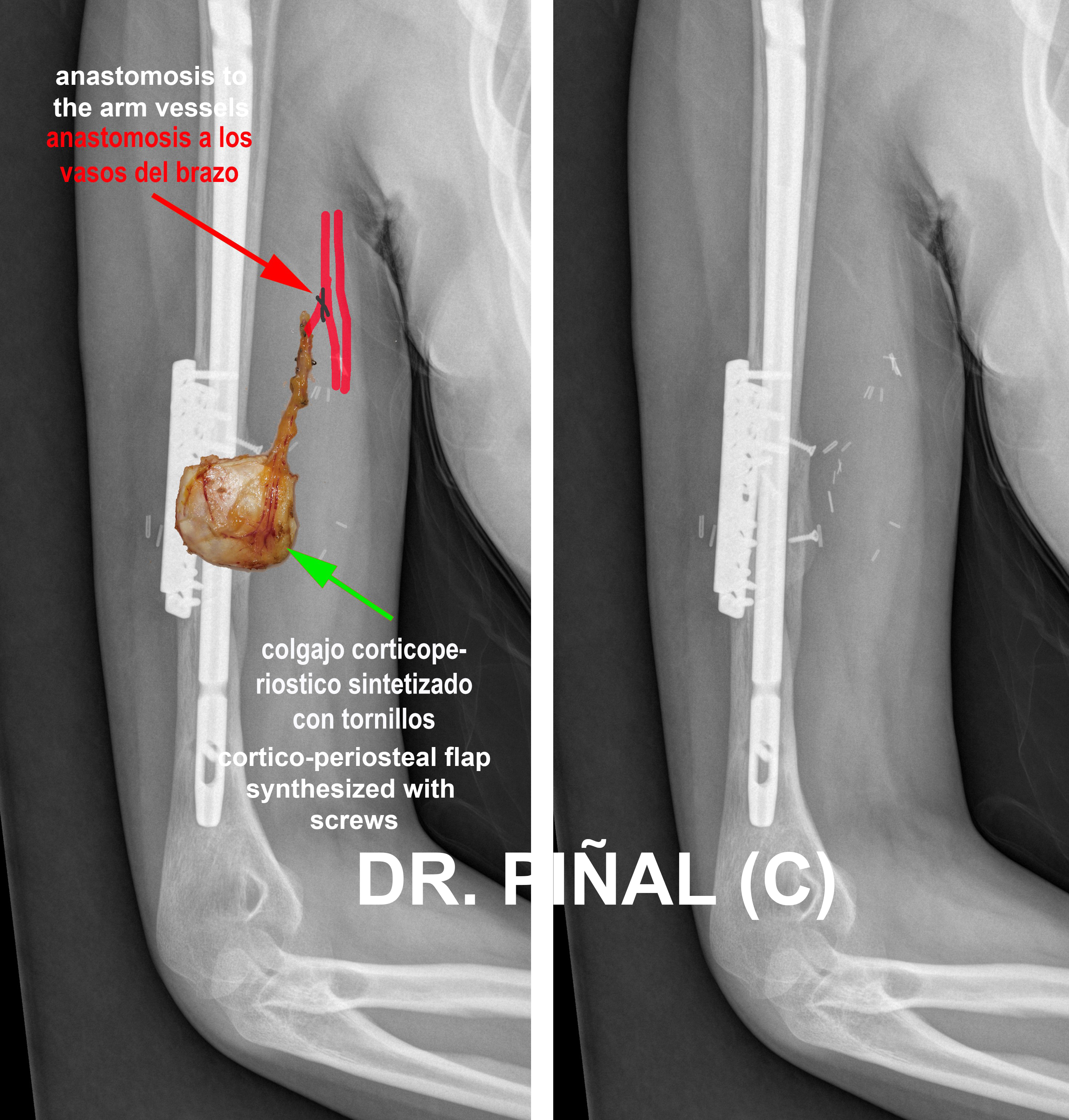
In turn, the osteosynthesis is reinforced with 2.7 mm plates and the flap is stabilized with two 2.0 mm compression screws. The rest of the bone defect is compacted with the cancellous (material from the interior of the bone taken from its end or epiphysis) that had also been taken from the femur previously.
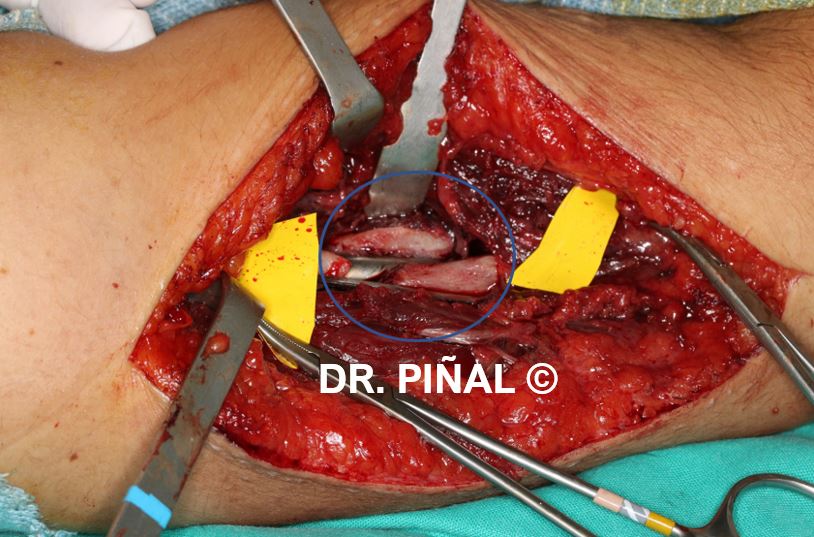

In the same operation, the 12 cm defect in the radial nerve is reconstructed with nerve grafts.
The results
The vascularization and regenerative capacity provided allow the bone to be fully consolidated in three months. Several months later, the recovery of the radial nerve is reinforced through tendon transplants, which help the patient to turn back to an almost normal function, which allows her to return to all her previous activities.
Dr Piñal and his team have more than 20 years of experience in long bone pseudarthrosis, with dozens of success stories. The Spanish surgeon has laid the foundations for the management of patients with crushing and consolidation failure with success rates of 99% (ref: ‘Vascularised corticoperiosteal grafts from the medial femoral condyle for difficult non-unions of the upper limb’, ‘Severe mutilating injuries to the hand: guidelines for organizing the chaos’, ‘Evolving concepts in the management of the bone gap in the upper limb. Long and small defects’, ‘Severe Crush Injury to the Forearm and Hand. The Role of Microsurgery’, etc.).
 es
es en
en fr
fr it
it ru
ru zh-hans
zh-hans